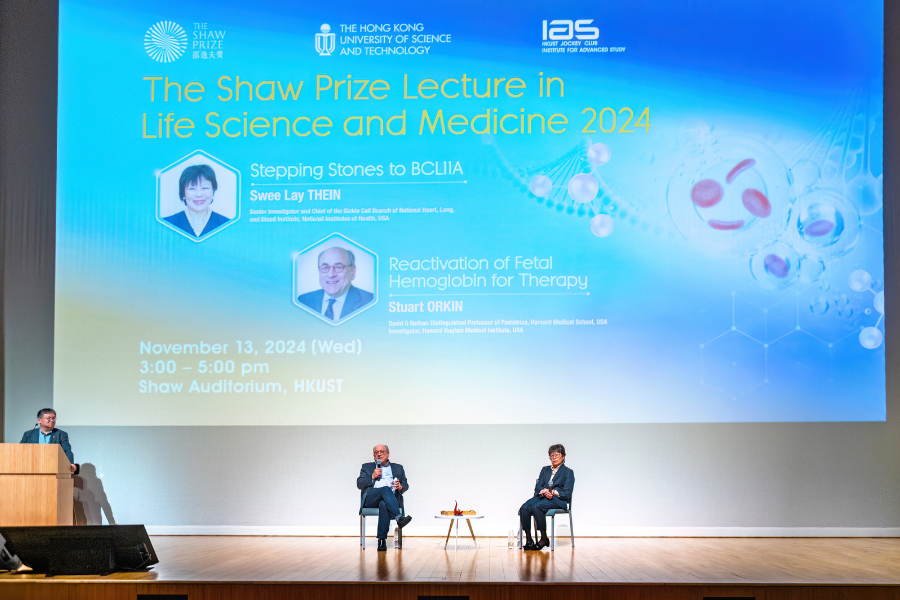
Stepping Stones to BCL11A / Reactivation of Fetal Hemoglobin for Therapy
Abstracts
Lecture by Dr. Swee Lay THEIN - Stepping Stones to BCL11A
Sickle cell disease (SCD) and β-thalassemia are the most common genetic disorders in the world and major sources of morbidity and mortality. For many years it had been known that patients with such disorders have milder forms of the disease when they produce higher levels of fetal hemoglobin (HbF), but it was not evident why the production of HbF was not suppressed in these patients as compared to the majority of adults. Early research focused on rare Mendelian mutations associated with hereditary persistence of fetal hemoglobin (HPFH), within the β-globin cluster, which led to the discovery of specific mutations that impair the fetal-to-adult hemoglobin switch. However, common HbF variability in the general population behaves as a complex quantitative trait with genetic factors accounting for approximately 89% of the variability. The first known quantitative trait locus (QTL) influencing HbF was the Xmn1–HBG2 site within the β-globin cluster, which demonstrated a modest but significant effect on HbF levels.
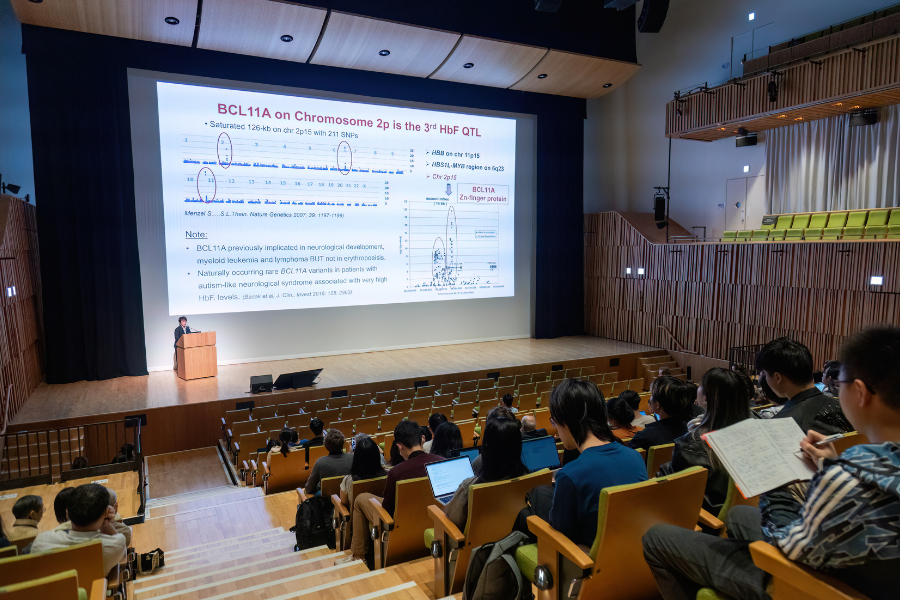
A major breakthrough, which involved genome-wide linkage and association studies, came with the identification of a QTL on chromosome 6q23–q24, encompassing the HBS1L–MYB intergenic region. Fine mapping and high-resolution association studies in diverse populations confirmed that this locus significantly influences HbF levels in both healthy individuals and patients with hemoglobinopathies. The advent of genome-wide association studies (GWAS) enabled the unbiased scanning of the entire genome for HbF-related loci. A pivotal GWAS targeting F-cell production in a European twin cohort revealed a novel QTL within intron 2 of the BCL11A gene on chromosome 2p15. This discovery was later replicated in a large Sardinian cohort, further implicating BCL11A alongside HBS1L–MYB and the β-globin cluster as major determinants of HbF levels. Subsequent studies validated the influence of BCL11A in various populations with SCD and β-thalassemia.
Discovery of the BCL11A gene as the key suppressor of fetal hemoglobin was transformative, enabling the development of treatments for ameliorating the clinical severity of SCD and β-thalassemia by inhibiting the expression of this gene to increase fetal hemoglobin.
Lecture by Prof. Stuart ORKIN - Reactivation of Fetal Hemoglobin for Therapy
Hemoglobin, which is the most abundant protein in red blood cells, carries oxygen throughout the body. In utero the developing fetus expresses a form of hemoglobin called fetal hemoglobin (HbF). Around the time of birth, expression of the g-globin subunit of HbF is progressively shut-off and accompanied by increasing expression of the b-globin subunit, resulting in production of adult hemoglobin (HbA). Mutations in the b-globin gene are responsible for the major hemoglobin disorders, b-thalassemia and Sickle Cell Disease (SCD), which are among of the most common diseases, affecting millions of individuals worldwide. More than 70 years ago, observation of families suggested that increased HbF lessens the severity of both disorders, and stimulated interest in how the switch from HbF to HbA is controlled and might be manipulated for clinical benefit. Prof. Orkin and his colleagues solved the puzzle of how the switch is controlled. They demonstrated that the protein BCL11A is the principal physiological regulator of the switch, and functions as a direct repressor of g-globin expression. Relying on common genetic variation in HbF levels among individuals, he and his colleagues identified a regulatory element (an enhancer) within the BCL11A gene itself that is required for BCL11A expression in developing red cells. With gene editing tools, they discovered that cutting of enhancer DNA at a single site greatly impairs BCL11A expression, thereby relieving repression of g-globin and resulting in increased HbF production. They proposed that gene editing of this site could be used to treat patients with SCD and b-thalassemia. This vision was carried forward by CrispR Therapeutics and Vertex Pharmaceuticals in clinical trials for these disorders, leading to approval of the first gene editing therapy (called Casgevy). The elegant studies of Prof. Orkin and his colleagues defined the mechanism of the fetal-adult hemoglobin switch and provide opportunities for future advancement of transformative therapy for millions of individuals.
About the Speakers
Dr. Swee Lay THEIN is currently Senior Investigator and Chief of the Sickle Cell Branch of National Heart, Lung, and Blood Institute at the National Institutes of Health, USA. She received her Bachelor’s degree in 1975 and obtained a DSc in 1999 from the University of Malaya, Malaysia. After her specialist training (1975–1982) and various clinical positions (1982–2000) in UK, she was appointed Professor of Molecular Haematology and Consultant Haematologist at King’s College London, UK (2000–2015). At the same time, she also served as Director of the Red Cell Unit at King’s College Hospital NHS Foundation Trust in London, UK. She was Head of the Division of Gene and Cell Based Therapy at King’s College London (2004–2010). She joined the National Heart, Lung, and Blood Institute at the National Institutes of Health in 2015 as Senior Investigator and Chief of the Sickle Cell Branch (2015–). She is a Fellow of the Academy of Medical Sciences, UK and the Academy of Life Sciences for Chinese in the UK.
Prof. Stuart ORKIN is currently David G Nathan Distinguished Professor of Pediatrics, Harvard Medical School, USA. He received his Bachelor’s degree from the Massachusetts Institute of Technology, USA in 1967 and obtained an MD from Harvard Medical School, USA in 1972. He was a Research Associate at the National Institutes of Health, USA (1973–1975) and Research Fellow in Pediatrics at Harvard Medical School, USA (1976–1978). At Harvard Medical School, he was successively Assistant Professor (1978–1981), Associate Professor (1981–1987), Leland Fikes Professor of Pediatric Medicine (1987–2003), David G Nathan Professor of Pediatrics (2000–2016) and David G Nathan Distinguished Professor (2017–). He also serves as an Investigator of the Howard Hughes Medical Institute and Principal Faculty Member of Harvard Stem Cell Institute. He is a member of the US National Academy of Sciences, the American Academy of Arts and Sciences and the American Philosophical Society.